Osteophyte
From Wikipedia, the free encyclopedia
| It has been suggested that Bone spur be merged into this article or section. (Discuss) |
| This article needs additional citations for verification. Please help improve this article by adding reliable references. Unsourced material may be challenged and removed. (December 2008) |
| Bone spur | |
| Classification and external resources | |
 | |
|---|---|
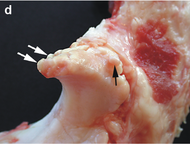
| Small marginal osteophytes (arrows) of the processus anconeus of the ulna can be seen in this gross pathological specimen of a sow. | |
| ICD-10 | M25.7, M77.9 |
| ICD-9 | 726.91 |
| DiseasesDB | 18621 |
| MeSH | D054850 |
Osteophytes, also known as bone spurs,[citation needed] are bony projections that form along joints.[1]
Contents[hide] |
[edit]Pathophysiology
Bone spurs form due to the increase in a damaged joint's surface area. This is most commonly from the onset of arthritis. Bone spurs usually limit joint movement and typically cause pain. [2]
Bone spurs form naturally on the back of spine as a person ages and are a sign of degeneration in the spine. In this case the spurs are not the source of back pains, but instead are the common symptom of a deeper problem. However, bone spurs on the spine can impinge on nerves that leave the spine for other parts of the body. This impingement can cause pain in both upper and lower limbs and a numbness or tingling sensations in the hands and feet due to the nerves supplying sensation to their dermatomes.[3]
Spurs can also appear on the feet, either along toes or the heel, as well as on the hands. In extreme cases bone spurs have grown along a person's entire skeletal structure: along the knees, hips, shoulders, ribs, arms and ankles. Such cases are only exhibited with multipleexostoses.
Osteophytes on the fingers or toes are known as Heberden's nodes (if on the DIP joint) or Bouchard's nodes (if on the PIP joints).
Bone spurs may also be the end result of certain disease processes. Osteomyelitis, a bone infection, may leave the adjacent bone with a spur formation. Charcot foot, the neuropathic breakdown of the feet seen primarily in diabetics, will also leave bone spurs which may then become symptomatic.
[edit]Cause
Osteophyte formation has been classically related to any sequential and consequential changes in bone formation due to aging, degeneration, mechanical instability, and disease. Often osteophytes form in osteoarthritic joints due to damage and wear from inflammation. Calcification and new bone formation can also occur in response to mechanical damage in joints, or at the attachment points for ligaments and tendons.[4]
Calcium is the most abundant mineral in the body but may also be the most deficient. The amount of calcium that we absorb from our food varies widely. Our age is one factor. An adolescent may absorb up to 75% of the calcium obtained from foods, while in adults the maximum absorption rate ranges from 20% to 30%.
Even though our bones feel solid and seem permanent they're just like any other body tissue - they're constantly being broken down and formed again. In an adult, 20 percent of bone calcium is withdrawn from bones and replaced each year. Thus, every five years the bones are renewed.
Calcium is found in the extra cellular fluids and soft tissues of the body where it is vital to normal cell functioning. Much of the calcium in soft tissues is concentrated in muscle, although it is contained in the membrane and cytoplasm of every cell.
When the body is deficient of calcium it begins to leach calcium from the bones. In many people this happens to be in the heel of the foot or some other weak area of the body. As the calcium is being leached, it forms an eruption (similar to a volcano). This eruption is the bone spur.
Many people that have suffered from bone spurs found relief when they properly supplemented their diet daily with "good" calcium.[citation needed] They found that providing their body with "good" calcium along with other vital minerals stopped the "leaching process" (calcium deficiency) thus allowing the bone spur to shrink down and eventually disappear.[citation needed] With the bone spur gone, the surrounding damage from the spur is able to heal also.[citation needed]
[edit]References
| This article needs references that appear in reliable third-party publications. Primary sources or sources affiliated with the subject are generally not sufficient for a Wikipedia article. Please add more appropriate citations from reliable sources. (May 2009) |
| This article contains weasel words, vague phrasing that often accompanies biased or unverifiable information. Such statements should be clarified or removed. (May 2009) |
- ^ osteophyte at Dorland's Medical Dictionary
- ^ Bone spurs MayoClinic.com
- ^ Laser Spine Institute
- ^ Nathan M, Pope MH, Grobler LJ (Aug 1994). "Osteophyte formation in the vertebral column: a review of the etiologic factors--Part II". Contemporary Orthopaedics 29 (2): 113–9. PMID 10150240.
[edit]External links
- Mayo Clinic website concise information on bone spurs
- Bone spur details, treatment, etc.
| ||
| ||


No comments:
Post a Comment